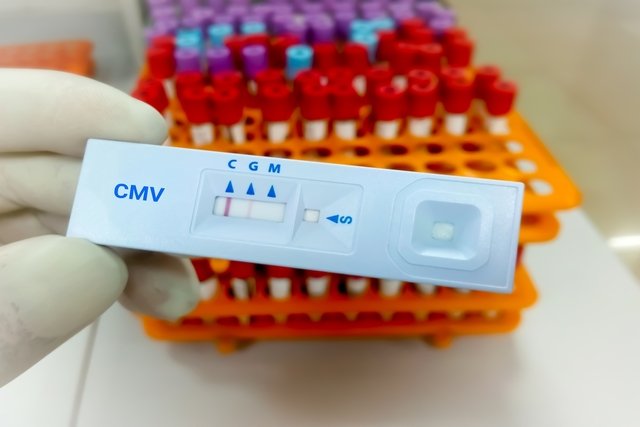
The IgG test for cytomegalovirus is a serological test that aims to assess whether a person has antibodies against the cytomegalovirus virus (CMV), which are normally formed after an infection with this virus. IgG is considered positive or reactive when the concentration of this antibody in the blood is equal to or greater than 1 U/mL.
This test is mainly indicated during pregnancy, and is normally carried out together with the IgM measurement, to find out if there is a past or recent infection and, therefore, to be able to start the most appropriate treatment, if necessary.
It is very important that this test is carried out in the first trimester of pregnancy, because if a woman becomes infected during this period, there is a greater chance of it being transmitted to the baby and leading to complications, such as microcephaly, congenital deafness and epilepsy, for example. . Despite being frequently requested during pregnancy, the IgG test for cytomegalovirus can be recommended for everyone, especially when there is suspicion of infection. Learn more about cytomegalovirus.
What does reagent IgG mean?
The IgG reagent result for cytomegalovirus indicates that the person has antibodies against the virus, which may have happened due to past or recent infection. Reference values for cytomegalovirus IgG may vary depending on the laboratory, however the serological test is considered positive or reagent when greater than or equal to 1 U/mL.
It is important to note that a positive result or IgG reagent does not necessarily indicate that the infection is active. To do this, it is important to carry out an IgM test for cytomegalovirus, as this immunoglobulin is the first to be produced when there is an infection. Learn more about IgM and IgG.
Worried about your exam results?
How to confirm cytomegalovirus infection
The symptoms of a cytomegalovirus infection are non-specific, including muscle pain, fever above 38ºC or sore tongue. Furthermore, in many cases there are no symptoms at all, as the virus can remain dormant for a long time. For this reason, the best way to confirm the infection is through a blood test, which must be recommended by your doctor.
What does the result mean
The diagnosis is made with the CMV blood test during pregnancy, the result may be:
- IgG greater than or equal to 1 U/mL: it is considered that the test is positive or reactive, and may indicate that the person came into contact with the virus through an old infection or had a recent infection, and it is important to evaluate the presence of IgM in the circulation to check whether the infection is active ;
- IgG less than 1 U/mL: it is considered that the test is negative or non-reactive, which may indicate that the person has never been in contact with the virus or has had an acute infection a few days ago, and it is important to assess the presence or absence of IgM;
- Non-reactive or negative IgM and reactive or positive IgG: the woman has had contact with the virus for a longer time and the risk of transmission is minimal.
- Reactive or positive IgM and non-reactive or negative IgG: acute cytomegalovirus infection is more worrying, the doctor should guide the treatment.
- Reactive or positive IgM and IgG: An avidity test must be performed. If the test is less than 30%, there is a greater risk of infection of the baby during pregnancy.
- Non-reactive or negative IgM and IgG: there has never been contact with the virus and, therefore, preventive measures must be taken to avoid possible infection.
When an infection is suspected in the baby, a sample of amniotic fluid can be taken to assess the presence of the virus. However, according to the Ministry of Health, the baby’s examination should only be carried out after 5 months of pregnancy and 5 weeks after the pregnant woman becomes infected.
How should the treatment be
Treatment for cytomegalovirus during pregnancy must be carried out according to the obstetrician’s guidance, with the use of antiviral medications, such as Acyclovir, for example, or injection of immunoglobulins, which aim to stimulate the immune system and combat infection, preventing transmission to the baby.
During treatment, the doctor must regularly recommend tests to monitor the baby’s development and ensure that the virus is not causing changes. Find out more details about the treatment of cytomegalovirus in pregnancy.
What to do to avoid infection during pregnancy
Since there is still no vaccine that helps protect against the virus, it is important that pregnant women follow some general recommendations to avoid infection, such as:
- Use a condom for intimate contact;
- Avoid going to public places with lots of people;
- Wash your hands immediately after changing a baby’s diaper or whenever you come into contact with the child’s secretions, such as saliva, for example;
- Do not kiss very young children on the cheek or mouth;
- Do not use objects that belong to the child, such as cups or cutlery.
Children are mainly responsible for transmitting cytomegalovirus, therefore, these recommendations must be followed by pregnant women throughout pregnancy, especially if they work with children.
Bibliography
- PREGNANCY BIRTH&BABY. Cytomegalovirus (CMV) during pregnancy. Available at: <https://www.pregnancybirthbaby.org.au/cytomegalovirus-cmv-during-pregnancy>. Accessed on March 12, 2019
- AMERICAN PREGNANCY. Cytomegalovirus (CMV) Infection. Disponível em: <https://americanpregnancy.org/pregnancy-complications/cytomegalovirus-infection/>. Acesso em 12 mar 2019
- CARLSON, Amanda et al. Cytomegalovirus Infection in Pregnancy: Should All Women Be Screened?. Obstetrics & Gynecology. Vol.3. 4.ed; 172-179, 2010

Sign up for our newsletter and stay up to date with exclusive news
that can transform your routine!
Warning: Undefined array key "title" in /home/storelat/public_html/wp-content/plugins/link-whisper-premium/templates/frontend/related-posts.php on line 12
Warning: Undefined array key "title_tag" in /home/storelat/public_html/wp-content/plugins/link-whisper-premium/templates/frontend/related-posts.php on line 13