It is not difficult to find matters and more stories talking about Monosodium Glutamate, but usually the bias used is that it would be a great food villain, causing various ills of life. Is it?
The big question is: Do you know what is Monosodium Glutamate? Really? Really?
What is Monosodium Glutamate (GMS)?
In a very simple way: it is a salt formed by the radical glutamate and an atom of sodium (Na). The substance can also present as glutamic acid and as free glutamate as well.
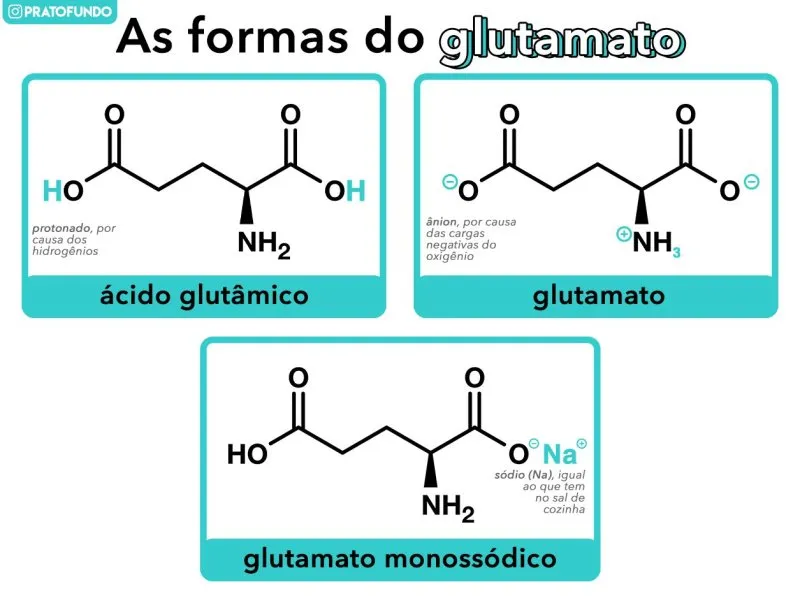
In the three versions that may exist, it is possible to note that the important part is the glutamate that is constant between the formats.
In the form of acid, it is an amino acid. That is, one of the blocks that together form the proteins that are part of practically all living beings, that is, it is part of life, day-to-day, food.
If the food is rich in protein, it will have glutamate. Within the physiology-biochemistry part, it is classified as non-essential, because the body can manufacture it.
And in the form of free glutamate (and anionic) is a neurotransmissorneurotransmitter: one or a set of substances that nerve cells (neurons) use to talk to each other. And it is the main and most abundant excitatory neurotransmitter.
Umami: The Fifth I Like
Another important function of glutamate: it is responsible for the stimulus that generates the fifth taste, the famous ummi. It’s hard to describe, but you can literally feel his presence. (In time: taste and taste are different concepts within Food Science)
Foods high in glutamate such as:
| Food | Free glutamate (mg/100g) | Glutamate bound (mg/100g) |
|---|---|---|
| Parmesan cheese | 1200 | 9847 |
| The Eggs and Eggs | 23 | 1583 Is a the |
| Chicken | 44 | 3309 |
| Meat | 33 . | 2346 I’s with |
| Tomatoes I mato | 140 | 238 |
| Peas and sheep | 5583 I’s the | 200 . |
| Soybean sauce | 782 | – – – the |
| Marmite . | 1960 | – – – the |
| Fish sauce nam-pla | 950 | – – – the |
Source: Monosodium Glutamate. The Safety Assessment. Technical report series 2003. No. 20 Food Standards Australia New Zealand.
In the table, the terms signifcam
- Free glutamate indicates that the glutamate radical is actually free, that is, it is not connected with other molecules and is not part of proteins.
- Glutamate bound: it is the opposite, that is, glutamate is connected with someone… either inside proteins and/or other substances.
The concept that glutamate was responsible for the perception of ummi taste was discovered by scientist Kikunae Ikeda in 1908 in Japan by studying broths made with seaweed that is one of the bases of Asian cuisine.
Despite being known for a long time, ummi was only recognized as a term to describe the stimulus generated by glutamate (and other substances such as guanosine and inosine) after the first ummi symposium held in Hawaii in 1985. And with the publication Umami: A Basic Taste (Kawamura and Kare) in 1987 that gathered the articles of the meeting.
At the symposium, Yamaguchi (1987) reported data on the response to the ummi/glutamate stimulus and showed that it does not overlap with other tastes (supply, sour, salty, bitter), implying that ummi is really different and is not a highlighter of the other basic tastes.
To be considered a basic taste it is necessary to meet certain criteria (KURIHARA, 2015):
- A basic taste should not be produced by combining other tastes.
- The basic taste is independent of the other tastes and should be proven by psychophysical and electrophysiological studies.
- Receptor specific to the basic taste must exist.
- The basic taste should be found in several foods.
The ummi already met several of the criteria, but still needed to identify which receptor was involved in perception. During the various studies, one of the starting points was the search for the same glutamate receptors that exist in the brain: mGluR1 and mGluR4. Remember? I said that glutamate is a neurotransmitter.
Several experiments were carried out to arrive in a response (consensus), from activating and blocking certain receptors. In the article by Li et al. (2002) reports and demonstrates that the T1R1+T1R3 receptors are responsible for the perception of the ummi stimulus. And the perception of ummi can be intensified with other substances such as guanosine and inosine.
A curious fact: versions of the common receptors in the brain (mGluR1 and mGluR4) were found in the tongue as well, but with a lower sensitivity to glutamate compared to the present in the brain tissue (SAN GABRIEL et al, 2005; CHAUDHARI, 2000).
Currently, the production of monosodium glutamate is made via bacteria of the genus Corynebacterium, especially Corynebacterium glutamicum when consuming carbohydrates (sugars). And in the past it has been used vegetable extracts and gluten as well.
Xenophobia against Asian immigrants
The bad reputation of glutamate is linked to xenophobia against Asian immigrants (especially Chinese) in the United States from an early age.
For example, in 1882 Chinese Exclusion Act was decreed, which prohibited the immigration of Chinese people solely based on racial issues. It was partially revoked only in 1943 and abolished in 1965. The political motivation for such an act is the same as we saw in the 20th centuries: immigrants “were robbed” (with many quotes here) jobs and opportunities of Americans.
And then when we entered the mid-40s, in World War II, the Japanese are on the target of discrimination. And the people who were American but from a Japanese family were forced to go to concentration camps inside the U.S. territory.
Other examples of tensions generated by racial issues: the motoring crisis in the 1980s that culminated in the murder of Vincent Chin in Michigan, and more recent in 2020-2021 because of the covid-19 pandemic.
Why talking about it is important? In addition to the obvious reasons, it generates context for the source of the whole trigger.
Complex symptoms of Monosodium Glutamate (Monosodic glutamate syndrome)
It all started because of a letter, this letter, not an experiment study in 1968.
A letter was sent to the New England Journal of Medicine (NEJM) by Dr. Robert Ho Man Kwok in 1968 reporting a number of symptoms-observations: numbness of the nape that follows to arms, palpitations and weakness in general after consuming Chinese dishes of Chinese cuisine.
For this reason, the term: Chinese Restaurant Syndrome syndrome and was also the title used in the magazine, but it is not possible to say who gave this name, the doctor or the editor of the magazine.
In 1995, the Federation of American Societies for Experimental Biology (FASEB) Federação das Sociedades AmericanasBiologia Experimentalproposed that it be called MSVo disease complexComplexo de sintomas de GMS. And depending on the source it is also called monosodium glutamate syndrome.
The letter (I read the original publication), the doctor explains in a very simple and casual way. And most importantly, it suggests several reasons and not just glutamate. Since the use of soy sauce, baking wine (cooking wine made of rice and very common in Chinese cuisine) because the effects are similar to alcohol poisoning, a large amount of sodium in the food (causing an imbalance of sodium in the tissues).
Finally, the doctor concludes by indicating that he has no experience in this type of research and passes the doubt on to colleagues in the area. And he would be more than willing to cooperate to seek a cause.
According to Lemesurier (2017), Kwok’s letter received answers, but was seen as a joke and not taken seriously by the community. However, the media took the assumption as fact and began writing about the dangers of glutamate.
Some of the materials had the following calls (LEMESURIER, 2017):
- Chinese Restaurant Syndrome Puzzles Doctors: New York Times in 1968.
- Four Scientists Find Chinese Food Fans Can Avoid Suffering (Four scientists discover that fans of Chinese food can avoid suffering): New York Times in 1969.
- Chinese Food Make you Crazy? MSG is No. 1 Suspect (Chinese food drives you crazy? MSG is suspect: Chicago Tribune in 1979.
Historian Ian Mosby wrote in the article “That Won Ton Soup Headache”: The Chinese Restaurant Syndrome, MSG and the Making of American Food, 1968–198 as glutamate was transformed into this goat-expiatory for something much worse: racism against sino-Americans. The belief in the harms of glutamate is:
product of a racialized discourse that framed much of the scientific, medical and popular discussion around the condition (…) that is rooted in certain fears and long-standing curiosities about an “orient” exotized
A prank and the turnaround
I comented earlier that the letter sent had been seen as a joke and the answers about it as well. So the problem is that the correspondence section of NEJM magazine was known for the jokes they sent there… and for some reason the magazine actually published.
In 2018, a year after the article was published, Jennifer Lemesurier received a voice message that could change everything (or could not) change: it was a message from another doctor Howard Steel who coincidentally was a student at Colgate University (and board member) where Lemesurier worked.
In the message, Steel reported that the letter sent to NEJM had been written by him as a form of joke and bet to see whether it would be published or not. The case was reported in two articles The Strange Case of Dr. Ho Man Kwok, signed by Michael Blanding and on This American Life in episode 668: The Long Fuse.
Steel told Blanding that even the signed name (Ho Man Kwok) was to be a tip that it was a joke: a somewhat questionable word game.
The terms “Ho” and “Man” would be to mean “human” (human, phonetics remember) and “Kwok” would be for “ crock” (in the sense of wrong, defective). The questionable part: it is a not very polite pun with surnames and words that look (or are) Chinese.
Steel’s story made sense and Lemesurier believed her. But for Blanding some points were not so clear and decided to research more. One of them was the workplace of such a character created: National Biomedical Research Foundation.
The place really existed and in it the – true ?!? – Dr. Robert Ho Man Kwok had worked. Lots of coincidences, right? After all, Steel said he created the name out of nothing. If the real Ho Man had not written the letter, he would have contacted the magazine to undo the misunderstanding as Blanding points out.
What happened in fact we will never know, because the characters of the story have already passed away. The real Robert Ho Man Kwok died in 2014, and Howard Steel in late 2018.
The twist: On This American Life program (interviewer Lilly Sullivan) contacted the family of Robert Ho Man Kwok to see if they knew anything. And… they confirmed that he had written the letter yes.
But it didn’t stop there, Sullivan needed to talk to one more person: Anna Steel, daughter of Howard Steel. She told her whole story, she grew up listening to the letter. For Anna, she believes in Kwok’s family, knowing the father she had. He liked to play plays for people and that would be his final prank. That is, make people believe that he had written the letter when he did not actually write.
What makes the story more absurd is that Howard Steel was a prominent doctor in his environment, doctor of anatomy, pioneered in surgical techniques, founded a pediatric treatment center for spinal cord injuries at the Philadelphia Shriners hospital. That is, it was not – per se – a person for nothing.
But is it bad or not?
Not a! No. But it does.
Since this story began there in the 1960s, studies to determine whether it actually existed or not were made. And as expected: there was no consensus.
Early studies have many planning failures or sampling was too limited. For example, Schaumburg (1969) reported symptoms in participants in several tests, but with a methodology that was not the best and the number of participants inconsistent.
The 2000 study Multicenter, double-blind, placebo-controlled, multiple-challenge evaluation of reported reactions to monosodium glutamate, published in the Journal of Allergy and Clinical Immunology is one of the most recent despite being over 20 years old that address the subject.
The question is not whether it does harm or not: whether consumed in normal amounts (read common sense) is not bad. The detail is: there may be people who feel some discomfort after consuming glutamate. How we learn in Pharmacy: the patient can be allergic even to the allergy drug.
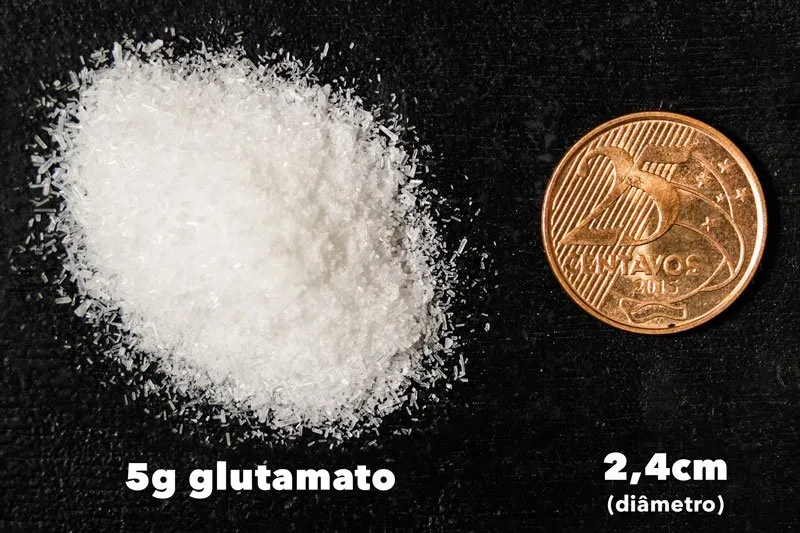
The article suggests that at high doses (5g of glutamate) may cause symptoms in some people within the protocol used in the experiment. For example, daily consumption of glutamate under normal conditions in European and Asian countries is around 0.3–1g and 1.2–1.7g, respectively.
Despite being one of the most robust studies published, there are still limitations in the planning of the experiment and in the execution of the experiment.
The selected participants had a predisposition or pre-conception that they were ill-like when they consumed glutamate, which may influence the test itself. Even though it was a double-blind experiment (neither the participants nor the researchers knew what samples were being administered) for ethical and transparency issues the participants know for what type of test they were recruited and sign a consent form.
Protocol A, participants were expected to be fasting and took a solution with 0 (placebo) or 5 grams of glutamate that had a citrus flavor to try to mask the ummi taste of glutamate. But in this amount, the ability of citric and acidic taste to mask glutamate is limited. (Note: 5g glutamate is enough to be consumed at once)
Thus, if the ummi taste is not masked correctly, the participant knows that the sample received has glutamate. Therefore, the pre-conception and auto-suggestion that it can do harm can influence the test response (it is the nocebo concept).
To try to eliminate a possible bias, the study had the C protocol in which only participants who presented symptoms for glutamate solution were chosen. And in this new test, the sample changed: it was an opaque capsule containing 5g glutamate or 5g of sucrose (sugar) along with 200mL of water.
And the participants who presented symptoms made the last protocol D in which the sample changed again, in addition to the glutamate capsule or sucrose was consumed a bowl of cereals (sucrilhos) with semi-skimmed milk.
The experiment had a good sampling at the beginning (n ? 130 participants) in the first phase (protocol A). But as it progresses, already in protocol B this number decreased because of the test criteria, which is expected. However, there were also withdrawals, out of the 86 that could participate, only 69, which is a small sample.
For protocol C, the sampling decreased again being only 12 participants and only 2 reported symptoms after ingestion of the glutamate capsule. And the article emphasizes, the symptoms reported by these two participants were not the same between protocols A and C.
In protocol D (which had cereal with milk), the two participants were tested 6 times: 3 times with placebo and 3 times with glutamate. And they only showed symptoms in only 1 of the glutamate tests. And again, the symptoms were not the same reported previously. Due to the limited number of participants, statistical treatment is impossible.
But it was just an article
I know the first question will be: but you only spoke / took an article ! Yes and no.
I actually researched several articles (see references below). The big question is: articles and/or experiments like this one of 2000, with almost all this rigor in the methodology do not exist or have not been published yet.
Although it is super interesting, it is not an urgent issue. Translation: is not something that impacts in a super negative way the life or health of the vast majority of people so that there is investment for this. Research requires funds (read money), and they usually go to projects that can benefit a larger group of people. That is not the case.
What we can assume today: that there may be people sensitive to glutamate and when they consume in large amounts of isolation and fasting can podeinduce uncomfortable symptoms, but without immediate risk for life/health.
The international agency (read type Anvisa, but from other countries) consider glutamate a safe substance (usually recognized as safe, GRAS).
Support the PlateFund
You help keep the site and videos on the air and we have very cool rewards, come to know how!
Very Long; Not Li
- No, it doesn’t hurt if you’re not allergic or sensitive to substance.
- Glutamate is naturally present naturalmentein several foods, within living things because it functions as an amino acid and neurotransmitter.
- Umami was recognized as the fifth taste in 1985, and the recipients responsible for the perception of the stimulus in 2002.
- The fuse of bad reputation was a letter in 1968 to the New England Journal of Medicine (NEJM) reporting some symptoms and giving several possible causes, not just glutamate.
- The scientific media did not give as much importance and treated it as a joke, as the section was correspondence of NEJM was known for this type of content.
- The general media took the idea and published it as if it were a fact and ended up spreading.
- The idea spread strongly because of racial issues, prejudice and economic tensions present in the United States against Asian immigrants, mainly Chinese.
- The evidence shows that symptoms can appear in very specific situations when consuming more than 3g of glutamate, in isolation, at once and fasting. Normal consumption during feeding in one day does not exceed 2g even in Asian countries.
- There are not so many researches with clinical experiments (read with humans), as it is not an urgent issue.
- Despite having articles that seek to clarify the subject, the oldest suffer from planning limitations and failures in execution. Even though the 2000 article is one of the most robust, presents limitation in the sampling of participants.
- The leading international regulatory agencies (American and European) consider glutamate as a safe substance when consumed for its basic purpose. And in Brazil, Anvisa also authorizes the use by RDC 239/2018.
- In short: you can eat, but do not eat pure and in excess (which serves everything in this life), in isolation or in a fasting way.
Bibliography
- Blanding, Michael. The Strange Case of Dr. Ho Man Kwok. Colgate Magazine, 2019.
- CHAUDHARI, Nirupa et al. The metabotropic glutamate receptor variants functions a taste receptor, Nature Neuroscience, vol. 3, no. 2, pp. 113–119, 2000.
- FENNEMA; Owen R. Fennema’s Food Chemistry. New York, 1996.
- FSANZ: Monosodium Glutamate. The Safety Assessment. Technical report series 2003. No. 20 Food Standards Australia New Zealand.
- GEHA, Raif S. et al. Multicenter, double-blind, placebo-controlled, multiple-challenge evaluation of reports reactions to monosodium glutamate. Journal of Allergy and Clinical Immunology, v. 106, issue 5, p. 973 – 980, 2000.
- IKEDA, Kikunae. On a new seasoning, Journal of the Tokyo Chemical Society, vol. 30, pp. 820–836, 1908.
- KAWAMURA, Yojiro; KARE, Morley. Umami: A Basic Taste, Marcel Dekker, New York, NY, USA, 1987.
- KAZMI, Zehra et al. Monosodium glutamate: Review on clinical reports, International Journal of Food Properties, 2017, 20:sup2, 1807-1815.
- KURIHARA, Kenzo. Umami the fifth basic taste: history of studies mechanisms on receptor and role as a food flavor. BioMed Research International, 2015, 2314-6133.
- LEMESURIER, Jennifer. Uptaking Race: Genre, MSG, and Chinese Dinner. Poroi, 2017.
- McGEE, Harold. On food and cooking: the science an lore of the kitchen. New York: Scribner, 2004.
- – MOSBY, Ian. That Won-Ton Soup Headache: The Chinese Restaurant Syndrome, MSG and the Making of American Food, 1968–1980, Social History of Medicine, Volume 22, Issue 1, April 2009, Pages 133–151.
- Nelson, David L., COX, Michael M. Lehninger Principles of Biochemistry. 5ed. New York: 2008.
- NONYE HENRY-UNAEZE, Helen. Update on food safety of monosodium l-glutamate (MSG), Pathophysiology, v. 24, issue 4, 2017, p.243-249.
- THE LONG FUSE. This American Life. Chicago: PRX The Public Radio Exchange, February 15, 2019. radio program.
- ROBERTS, A. et al. Risk Assessment Paradigm for Glutamate. Ann Nutr Metab 2018;73(suppl 5):53-64.
- SAN GABRIEL, Anna et al. Cloning and characterization of a novel mGluR1 variant from vallate papillae that functions a receiver for L-glutamate stimuli. Chemical Senses, vol. 30, pp. i25–i26, 2005.
- SANO, Chiaki. The History of glutamate production. The American journal of clinical nutrition vol. 90,3 (2009): 728S-732S.
- SCHAUMBURG, Herbert. H. et al. Monosodium L-Glutamate: Its Pharmacology and Role in the Chinese Restaurant Syndrome. Science 1969, 163 (3,869), 826–828.
- Walker, R., LUPIEN, J. R. R. The Safety Evaluation of Monosodium Glutamate, The Journal of Nutrition, v. 130, issue 4, april 2000, p. 1049S–1052S.
- ZANFIRESCU, Anca. et al. A Review of the Alleged Health Hazards of Monosodium Glutamate. Comprehensive Reviews in Food Science and Food Safety, 2019, 18: 1111-1134.
- Analysis of adverse reactions to monosodium glutamate (MSG). Federation of American Societies for Experimental Biology Publisher, American Institute of Nutrition, 1995: 1-119.

Sign up for our newsletter and stay up to date with exclusive news
that can transform your routine!
Warning: Undefined array key "title" in /home/storelat/public_html/wp-content/plugins/link-whisper-premium/templates/frontend/related-posts.php on line 12
Warning: Undefined array key "title_tag" in /home/storelat/public_html/wp-content/plugins/link-whisper-premium/templates/frontend/related-posts.php on line 13