Hip osteoarthritis, also called osteoarthrosis or coxarthrosis, is wear and tear on the joint that causes symptoms such as localized pain in the hip, a feeling of sand when moving the joint and a tingling sensation in the legs, which appears mainly during the day and when walking or remain seated for a long time.
This disease causes degeneration of the cartilage, and it is very common to appear in the hip, as it is a region that supports much of the body’s weight and is always in movement and, generally, happens in people over 45 years of age, but it can also happen in younger people, especially in the case of athletes who use their joints a lot.
Treatment must be guided by an orthopedist, and consists of relieving symptoms with the use of medication and physiotherapy. Surgery can be performed as a last resort, when there is no improvement with clinical treatment, performed by scraping the inflamed part or replacing the cartilage with a hip prosthesis.

Symptoms of hip osteoarthritis
The most common symptoms of hip osteoarthritis include:
- Hip pain, which worsens when walking, sitting for a long time or lying on one side on the affected joint;
- Walking with a limp, needing a cane to better support the body weight;
- Feeling of numbness or tingling in the legs;
- The pain can range from the hip to the knee on the inside of the leg;
- Burning pain in the leg;
- Difficulty moving the leg in the morning;
- Feeling of sand when moving the joint.
- Difficulty cutting toenails, putting on socks, tying shoes or getting up from a lower chair, bed or sofa.
This disease is caused by wear and tear on the hip joint, generally in genetically predisposed people, which occurs with advanced age, but hip osteoarthritis can also appear in young people, due to local trauma caused by sports, such as running and weight lifting, for example. Learn about other diseases that can cause hip pain.
Does hip osteoarthritis retire?
In some people, symptoms can be so intense that they can disable daily activities and even be a reason for retirement. But, to avoid this, it is necessary to strictly follow treatment and medical monitoring.
How to confirm the diagnosis
The diagnosis of hip osteoarthritis is made by the orthopedic doctor after evaluating the symptoms and checking the hip X-ray. Some words that may be written on the X-ray report and that suggest hip osteoarthritis are: narrowing of the joint space, subchondral sclerosis, marginal osteophytes, cysts or geodes.
Other tests that the doctor may order are computed tomography, which can tell if there is a bone tumor, and magnetic resonance imaging, which can be used to assess the condition of the head of the femur.
Possible causes
Hip osteoarthritis occurs due to the natural wear and tear of this joint, due to age, or due to frequent trauma, such as long-distance running, for example. In these cases, the head of the femur, which fits perfectly into the acetabulum of the hip, no longer fits completely. The joint surface becomes irregular and rough, and gives rise to osteophytes, which causes pain and decreased ability to move.
Some situations that favor the onset of hip osteoarthrosis are:
- Rheumatoid arthritis,
- Ankylosing spondylitis;
- Diabetes;
- Septic arthritis;
- Hip dysplasia;
- Local trauma or repeated trauma (running).
Therefore, it is important to keep these situations under control to eliminate pain and prevent the progression of osteoarthritis.
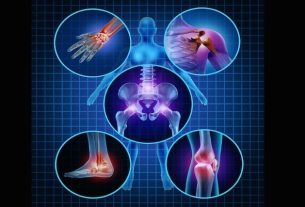
It is very common for a person who has osteoarthritis in one place to have it in others as well, such as the knees or shoulders, for example. Find out, in more detail, what causes it and what to do in case of osteoarthritis.
How the treatment is carried out
The main forms of treatment are:
1. Changes in habits
Some changes that may be useful for relieving pain and worsening the condition are reducing the frequency or intensity of physical activity that is causing osteoarthritis, reducing weight and using a cane, always supporting it in the hand opposite to the side of the pain. to reduce hip overload.
2. Medicines
Analgesic medications, prescribed by the doctor, such as dipyrone or paracetamol, can be used up to 4 times a day to alleviate symptoms. When symptoms are very intense, more powerful analgesics can be used, such as tramadol, codeine and morphine, in addition to injecting corticosteroids directly into the hip.
Anti-inflammatories, such as diclofenac and ketoprofen, or corticosteroids, such as prednisone, are only indicated during periods of worsening symptoms, and should not be taken routinely, due to the risk of causing kidney damage and stomach ulcers.
It is still possible to use supplements such as hydrolyzed collagen, glucosamine or chondroitin, which work to help renew cartilage and improve osteoarthritis in some people.
3. Physiotherapy
Physiotherapy treatment can be done with the use of devices that relieve pain, use of thermal bags, massages, manual traction and exercises, to improve range, lubrication and function of the joint, and must be done daily or at least 3 times per week.
4. Exercises
Exercises, such as water aerobics, Pilates, cycling or other exercises that do not worsen pain are important to strengthen muscles and protect the body’s joints. Therefore, it is recommended to strengthen the thigh muscles and do stretching and functional exercises.
The exercises can be started with elastic bands, but it is important to increase the level of difficulty using weights that can weigh up to 5kg on each leg.
5. Surgery
Surgery for osteoarthritis should be performed when other treatments are not sufficient to control the pain. It consists of removing the damaged cartilage partially or completely, and, in some cases, it is necessary to replace it with a hip prosthesis.
After the procedure, it is necessary to rest for around 10 days, which varies according to each person’s needs. In cases where a hip prosthesis is placed, recovery takes longer, and it is necessary to continue with physiotherapy for around 1 year or more, so that the movements are recovered in the best way. See what to do to speed up recovery after hip replacement.

Sign up for our newsletter and stay up to date with exclusive news
that can transform your routine!
Warning: Undefined array key "title" in /home/storelat/public_html/wp-content/plugins/link-whisper-premium/templates/frontend/related-posts.php on line 12
Warning: Undefined array key "title_tag" in /home/storelat/public_html/wp-content/plugins/link-whisper-premium/templates/frontend/related-posts.php on line 13