Malaria is a disease caused by the parasite Plasmodiumwhich causes symptoms such as fever, sweating, chills, nausea, vomiting, headache and weakness, and which is transmitted to people through the bite of an infected female mosquito Anopheles.
As it is transmitted by mosquito bites, the best way to prevent malaria is to avoid being bitten, through measures such as using repellent, placing protection on windows or wearing long-sleeved clothing, for example.
Malaria can be cured, but it is important that treatment is started quickly, as in many cases the disease can become serious, with anemia, reduced platelets, kidney failure or even brain damage, in which the chances of complications and death are greater.

Main symptoms
The main symptoms of malaria are:
- High fever, which may come and go in cycles;
- Sweats and chills;
- Strong headache;
- Nausea and vomiting;
- Muscle pain throughout the body;
- Weakness and constant tiredness;
- Cough and difficulty breathing.
In general, malaria symptoms appear between 8 and 14 days after transmission of the parasite, but in some cases they can take up to 30 days to appear, depending on the multiplication rate of the malaria protozoan and the person’s immune system.
Most of these symptoms are common to other diseases, so the best way to confirm malaria infection is to see a doctor, especially if you have been to a place with a malaria outbreak or where malaria is common, as is the case in the region. Amazon or Africa, for example.
Don’t ignore the signs your body is giving you!
How transmission happens
Malaria is only transmitted through the bite of a female mosquito. Anopheles infected person, who acquired the parasite by biting another person infected with the disease. This means that malaria is not contagious, that is, it is not transmitted from one person to another, except in very rare cases of sharing infected syringes or needles, poorly controlled transfusions and/or childbirth.
Generally, mosquitoes bite people during the evening or dusk. The places with the greatest risk of contamination are South America, Central America, Africa and part of Asia, mainly in places with clean water with little current, humidity and temperatures between 20º and 30ºC. In Brazil, the states most affected by malaria are Amazonas, Roraima, Acre, Tocantins, Pará, Amapá, Mato Grosso, Maranhão and Rondônia.
Malaria cycle
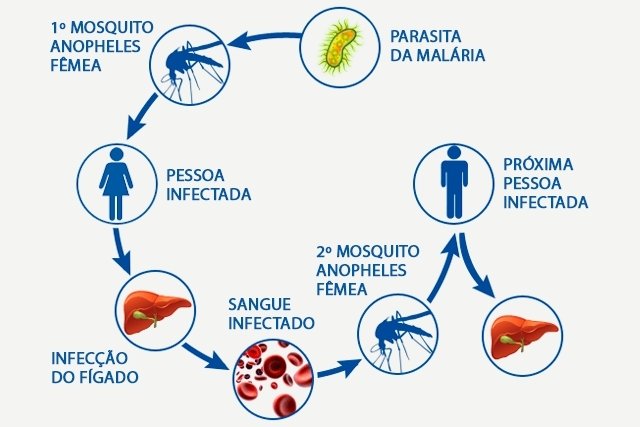
The parasite cycle Plasmodium in the human body it happens as follows:
- The bite of a female mosquito Anopheles transmits, through its saliva, the Plasmodium into the person’s bloodstream, in its Sporozoite phase;
- The sporozoites go to the liver, where they mature and multiply for about 15 days, giving rise to the form of Merozoites;
- Merozoites break through the liver cells and reach the bloodstream, starting to invade red blood cells;
- Inside the infected blood cells, which are called Schizonts, the parasites multiply and rupture this cell, and begin to invade others, in a cycle that lasts from 48 to 72 hours.
Within each schizont, the cycle varies according to the species of the Plasmodiumbeing 48 hours for species P. falciparum, P. vivaxe P. ovale and from 72 hours to P. malariae. During the period in which the red blood cells are ruptured and the schizonts become free in the blood, symptoms may become more pronounced, especially fever and chills.
How to confirm the diagnosis
The diagnosis of malaria is made by microscopic analysis of the blood test, also known as a thick drop. This test must be available at the health center or hospital, especially in areas most affected by malaria, and is carried out whenever symptoms indicative of the infection appear.
Furthermore, new immunological tests have been developed to facilitate and speed up the confirmation of malaria. If the result indicates that it really is malaria, the doctor may also order other tests to monitor and evaluate possible complications, such as a blood count, urine test and chest X-ray.
How the treatment is carried out
Malaria is treated with antimalarial drugs, such as Chloroquine, Primaquine, Artemether and Lumefantrine or Artesunate and Mefloquine, for example, which act by destroying the Plasmodium and preventing its transmission.
The chosen medications, doses and duration are indicated by the doctor according to age, severity of the disease and analysis of health conditions. Children, babies and pregnant women need special treatment, with Quinine or Clindamycin, always in accordance with medical recommendations and, generally, hospitalization is indicated.
It is also recommended:
- Eat normally, but avoid consuming fatty foods and increase protein consumption;
- Do not consume alcoholic beverages;
- Do not stop treatment even if symptoms disappear, due to the risk of recurrence and complications of the disease;
- Drink plenty of fluids during the day.
Malaria treatment must be started as soon as possible, as it can progress seriously and, without adequate treatment, can lead to death. Find out more about how the treatment is carried out to recover faster.
Possible complications
Complications of malaria usually happen when the disease is not treated properly or when the person has a weakened immune system, and can include:
1. Pulmonary edema
It happens when there is an excessive accumulation of fluid in the lungs and is more common in pregnant women, being characterized by faster and deeper breathing, and high fever, which can result in Adult Respiratory Distress Syndrome.
2. Jaundice
It arises due to the excessive destruction of red blood cells and damage to the liver caused by the malaria parasite, resulting in an increase in the concentration of bilirubin in the bloodstream, which results in the yellowish color of the skin, known as jaundice.
Furthermore, when jaundice is severe, it can also cause a change in the color of the whites of the eyes. Find out more about jaundice and how it is treated in these cases.
3. Hypoglycemia
Due to the excess of parasites in the body, the glucose available in the body is consumed more quickly, resulting in hypoglycemia. Some symptoms that may indicate low blood sugar include dizziness, palpitations, tremors and even loss of consciousness.
4. Anemia
When in the bloodstream, the malaria parasite can destroy red blood cells, preventing them from functioning properly and transporting blood to all parts of the body. Therefore, it is possible for a person with malaria to develop anemia, with symptoms such as excessive weakness, pale skin, constant headache and even a feeling of shortness of breath, for example.
See what to eat to prevent or treat anemia, especially if you are already being treated for malaria.
5. Cerebral malaria
In rarer cases, the parasite can spread through the blood and reach the brain, causing symptoms such as very intense headache, fever above 40ºC, vomiting, drowsiness, delirium and mental confusion.
How to protect yourself
Malaria prevention can be done through:
- Wearing light-colored and thin-fabric clothingwith long sleeves and long pants;
- Avoid areas most prone to contamination of illness, especially during dusk or dawn;
- Use DEET-based repellent (NN-diethylmetatoluamide), respecting the manufacturer’s guidelines regarding repellent replacement;
- Install protective screens against mosquitoes in windows and doors;
- Avoid lakes, ponds and rivers in the late afternoon and at night.
Anyone traveling to a place where there are cases of malaria can receive prevention treatment, called chemoprophylaxis, with antimalarial drugs, such as Doxycycline, Mefloquine or Chloroquine.
However, these medicines have strong side effects, which is why the doctor usually recommends this type of prevention for people who are at greater risk of developing a serious illness, such as going to places with high transmission rates or when the person has a disease that can have greater complications. with the infection.
These medications should only be used after medical advice and are generally started 1 day before the trip and persist for a few more days or weeks after returning.

Sign up for our newsletter and stay up to date with exclusive news
that can transform your routine!
Warning: Undefined array key "title" in /home/storelat/public_html/wp-content/plugins/link-whisper-premium/templates/frontend/related-posts.php on line 12
Warning: Undefined array key "title_tag" in /home/storelat/public_html/wp-content/plugins/link-whisper-premium/templates/frontend/related-posts.php on line 13



