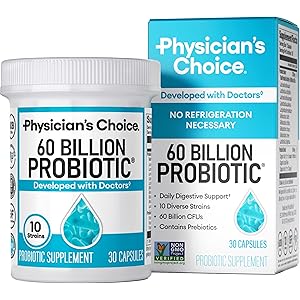
Physician's Choice Probiotics 60 Billion CFU - 10 Strains + Organic Prebiotics - Immune, Digestive & Gut Health - Supports Occasional Constipation, Diarrhea, Gas & Bloating - for Women & Men - 30ct
$23.97 (as of October 26, 2025 22:08 GMT +00:00 - More infoProduct prices and availability are accurate as of the date/time indicated and are subject to change. Any price and availability information displayed on [relevant Amazon Site(s), as applicable] at the time of purchase will apply to the purchase of this product.)Understanding IPV in Obstetrics
IPV, or Intimate Partner Violence, is a critical issue that affects many individuals during pregnancy and childbirth. In obstetrics, it is essential to recognize the signs and implications of IPV, as it can significantly impact maternal and fetal health. Healthcare providers must be trained to identify and address IPV to ensure the safety and well-being of both the mother and the unborn child.
The Impact of IPV on Maternal Health
Maternal health can be severely compromised by IPV. Women who experience violence from their partners may face a range of physical and psychological issues, including depression, anxiety, and increased risk of complications during pregnancy. Understanding the relationship between IPV and maternal health outcomes is vital for obstetricians and midwives to provide appropriate care and support.
Screening for IPV in Prenatal Care
Screening for IPV should be a routine part of prenatal care. Obstetric providers are encouraged to ask about IPV during initial visits and throughout the pregnancy. Effective screening tools can help identify women at risk, allowing for early intervention and support. It is crucial to create a safe environment where patients feel comfortable disclosing their experiences with IPV.
Effects of IPV on Fetal Development
IPV can have detrimental effects on fetal development. Exposure to violence can lead to low birth weight, preterm birth, and developmental delays. The stress experienced by the mother can also affect the fetus, highlighting the importance of addressing IPV in obstetric care. Understanding these risks can help healthcare providers advocate for the health of both mother and child.
Support Systems for Victims of IPV
Establishing support systems for victims of IPV is crucial in obstetrics. Healthcare providers should be knowledgeable about local resources, such as shelters, counseling services, and legal assistance. Providing information about these resources can empower women to seek help and make informed decisions regarding their safety and health.
Legal and Ethical Considerations in IPV Cases
Obstetricians and healthcare providers must navigate complex legal and ethical considerations when dealing with IPV cases. Mandatory reporting laws may require providers to report suspected cases of IPV, while also ensuring patient confidentiality. Understanding these legal frameworks is essential for providing ethical care and protecting the rights of patients.
Training Healthcare Providers on IPV
Training healthcare providers on IPV is essential for improving outcomes in obstetrics. Educational programs should focus on recognizing signs of IPV, effective communication strategies, and intervention techniques. By equipping providers with the necessary skills and knowledge, they can better support patients experiencing IPV and improve overall care quality.
Community Awareness and IPV Prevention
Community awareness plays a significant role in IPV prevention. Public health campaigns can educate individuals about the signs of IPV and available resources. By fostering a supportive community environment, we can reduce stigma and encourage victims to seek help, ultimately improving health outcomes in obstetrics.
Research and Future Directions in IPV and Obstetrics
Ongoing research is vital to understanding the complexities of IPV in obstetrics. Studies focusing on the long-term effects of IPV on maternal and child health can inform best practices and interventions. Future directions should include developing comprehensive care models that integrate IPV screening and support into routine obstetric care.